Pectus implants
A surgical technique used to treat most forms of pectus excavatum it involves placing an implant under the skin, soft tissue and muscle layer in front of the breast bone to mask the deformity. Compared to other types of surgery which correct the deformity it is a minor less invasive surgical procedure.
Previously the results of such implants were variable depending on patient selection, technique used and implant inserted. More recently, custom-made implants based on 3D reconstructive technologies have been developed which significantly improve on the cosmetic result.
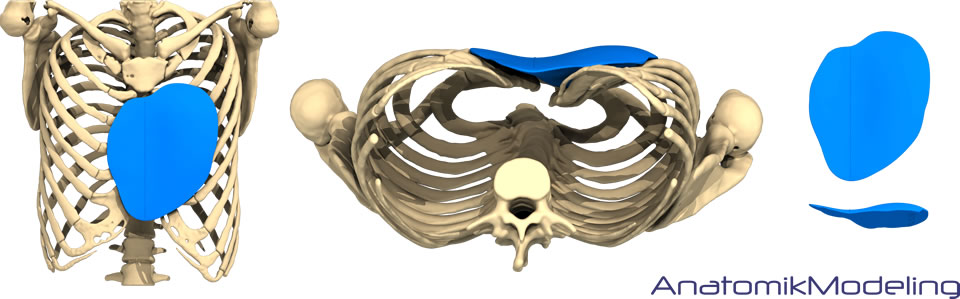
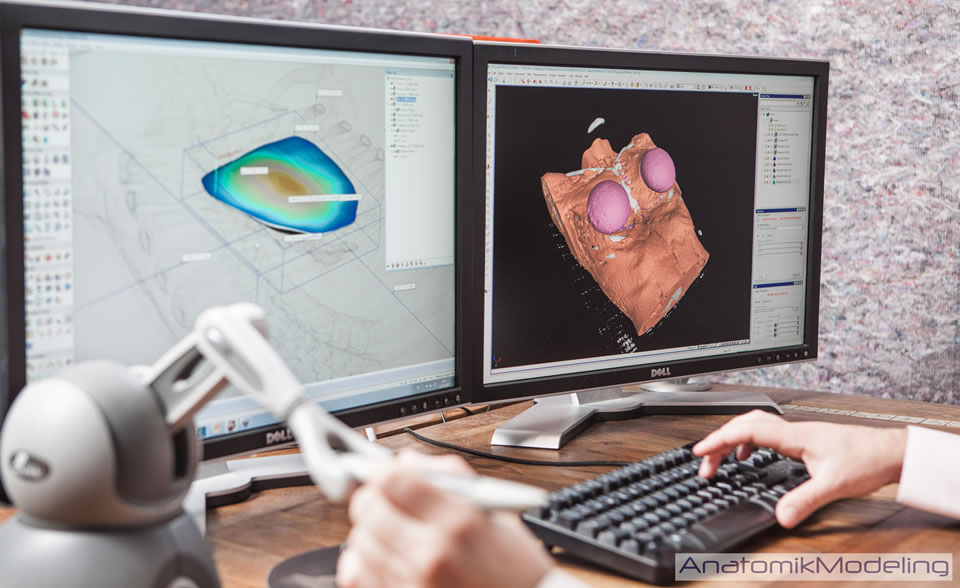
Using the latest 3D CT technology an implant is designed using an exact virtual anatomical model of the patient's chest deformity
Please click on the buttons below to see and read about patients verified experiences (in their own words) and testimonials (which generally include before and after treatment photos). The pectus clinic is very grateful to all the patients who provided feedback.
Working with AnatomikModeling, one of the world's leading 3D custom-made pectus implant experts the pectus clinic arranges for a virtually designed pectus implant created from each patient's 3D-scanned body to be made. Each implant is unique and perfectly fitted to each patient's anatomy.
Following expert assessment of your pectus deformity, if pectus implant surgery is considered the best option for you, the Pectus Clinic works with Mr David Gateley, an experienced plastic surgeon and founder of drg-plastic surgery.
A prosthetic pectus implant is a less intrusive non-corrective procedure, with generally quicker recovery time. It offers an alternative to more invasive corrective surgery particularly in patients with no symptoms or functional problems.
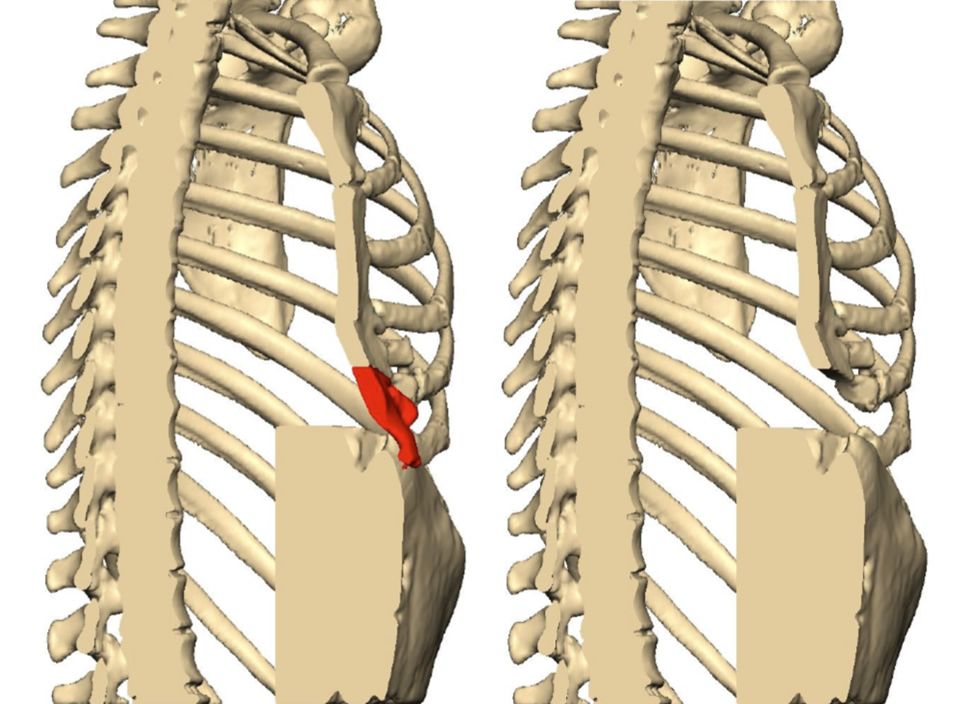
CT reconstruction highlighting area of residual pectus excavatum with protrusion (in red) before (left) and after excision (right) in a patient with unsatisfactory pectus excavatum chest wall correction (modified Ravitch) performed elsewhere
The custom made implants corrects the pectus excavatum and can be combined with breast implantation to augment small breasts or be used in patients with significant chest wall deformities such as those with Poland's syndrome.


Photos before (left) and 3 weeks following non-corrective surgery with pectus implant (right)
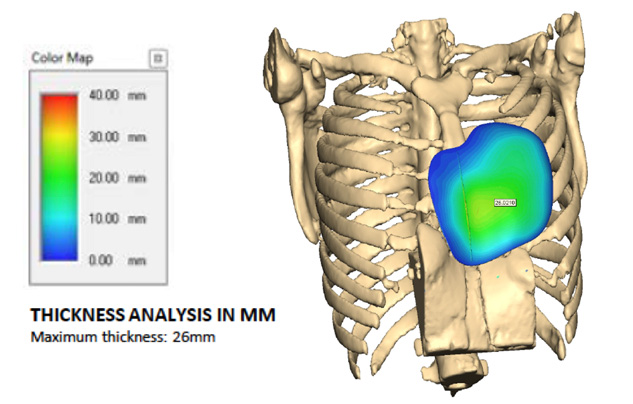
Chest CT reconstruction and 3D implant demonstrating graded thickness
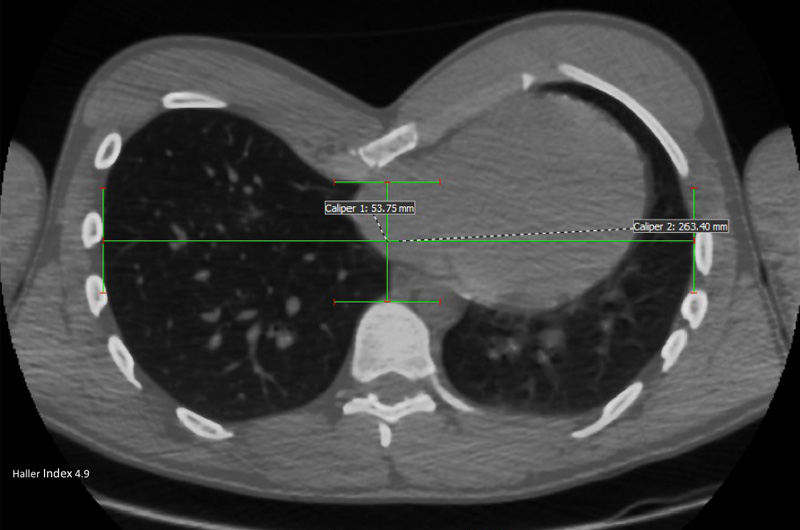
Chest CT showing a significant pectus excavatum
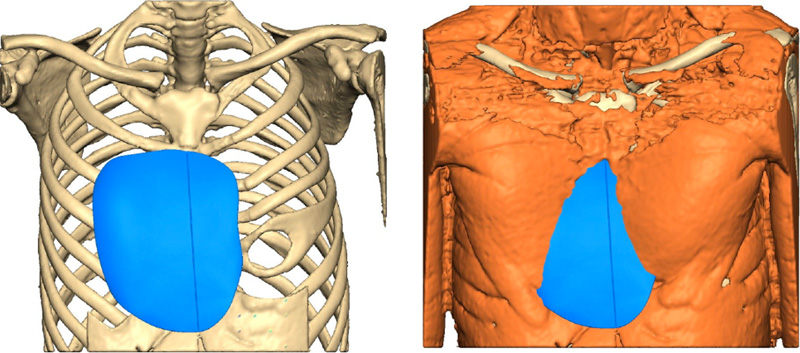
Front bony view and with muscle showing implant in place


Before (left image) and 6 weeks following non-corrective surgery with a pectus implant (right image)
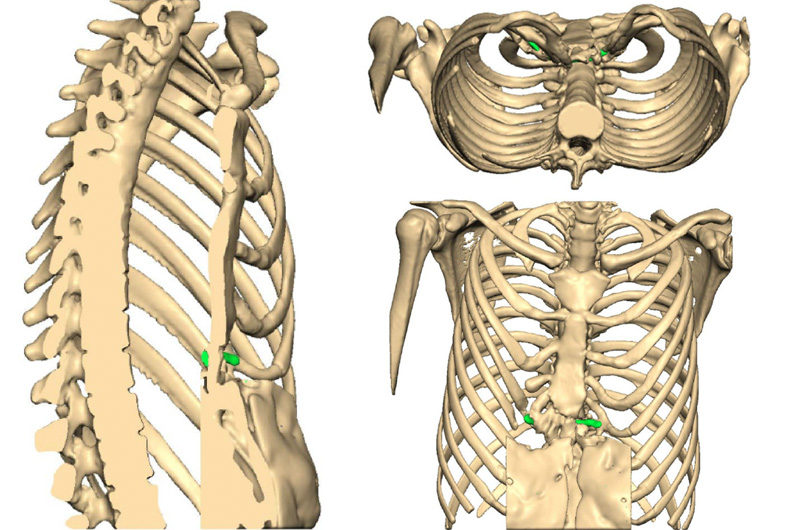
Chest CT reconstructions of chest with the mesh used to ‘hold’ sternum forward highlighted in green

Chest CT showing a significant residual pectus excavatum
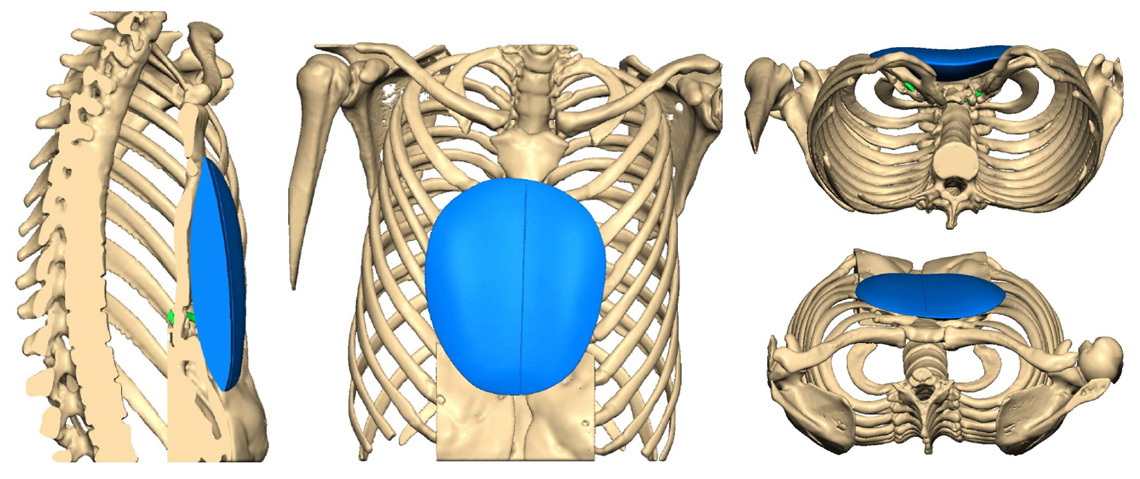
Chest CT reconstructions and planning scans of implant and it’s position in the chest




Before and 8 weeks following non-corrective surgery with a pectus implant. The implant was inserted through the previous scar
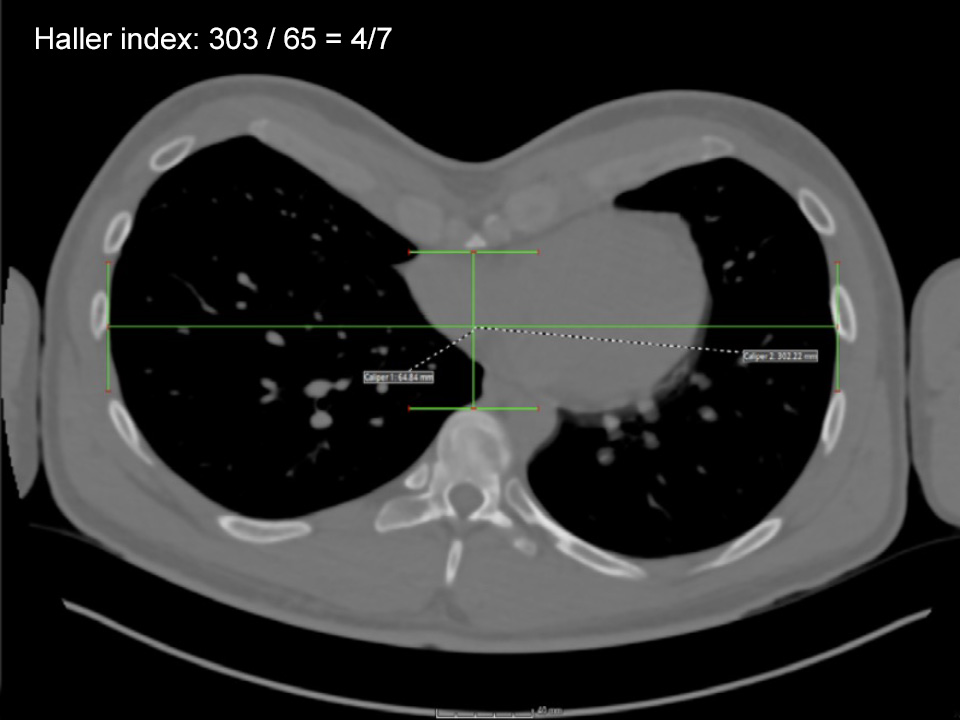


Chest CT showing severity of the pectus excavatum with Before and 12 weeks After non-corrective pectus excavatum surgery with a pectus implant. The implant was inserted through a small vertical scar made at the front of the chest. Note the patient had previously used the Vacuum Bell to try and improve the shape of his chest (causing skin discolouration on the Before photo). The Pectus clinic generally does not recommend using Vacuum Bell Therapy in older [adult] patients as there is little evidence it is effective.
Frequently Asked Questions about pectus implants for treatment of pectus excavatum
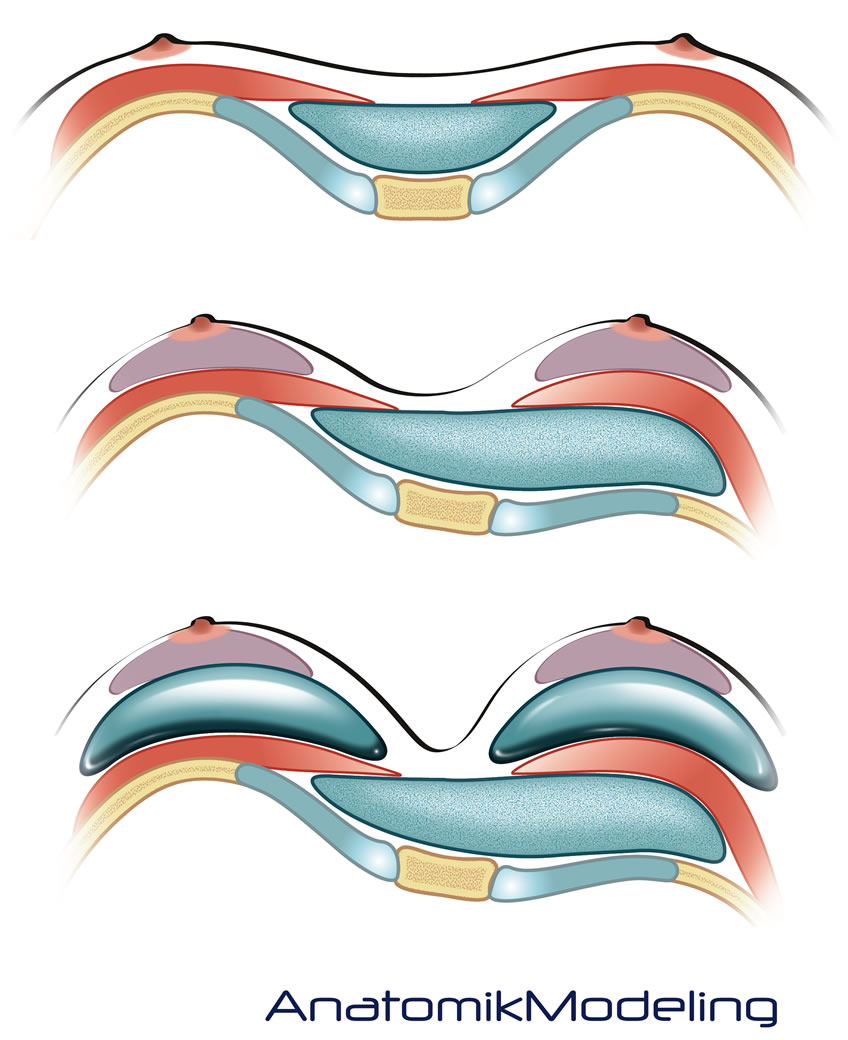
It is the insertion of a silicone implant behind the skin and soft tissues in front of the breast bone and rib cage in the dip or hollow created by the pectus excavatum.
Yes, it requires a general anaesthetic (being asleep) and takes about one hour to perform in most patients. It is regarded as a minor operation and it does not correct the underlying chest wall deformity but simply fills the dip so that the chest looks normal.
Maybe, but the uniqueness of the Pectus Clinic is that you will meet Mr Ian Hunt, a consultant thoracic (chest) surgeon knowledgeable about all types of pectus surgery, both non-corrective surgery such as this as well as corrective chest wall surgery. If deemed suitable and following a chest CT a second consultation with Mr David Gateley, an experienced cosmetic and implant surgeon who works with the Pectus Clinic will be arranged.
Good Question, it depends on several factors:
Firstly, you don’t like how your chest looks but do you want the chest wall deformity corrected (which is done by bringing the breast bone forward surgically) or not. That decision is often based on whether you feel the pectus excavatum is causing symptoms. If you are unsure, cardiac and respiratory investigations may help to see if your pectus excavatum is associated with ‘functional’ (affecting your health) problems. If not then a pectus implant, a non-corrective less invasive procedure may be right for you.
Secondly, if you are considering surgery for your pectus excavatum what sort of recovery period is acceptable to you. Pectus implant surgery is far shorter and associated with less pain.
Thirdly, what are the associated risks of surgery. Risks of surgery tend to increase with age and so a Pectus implant may be more appropriate in older patients where the risks of corrective chest wall surgery may be greater. Finally, and related to risks, if you have had previous corrective pectus surgery (a Nuss or modified Ravitch) but are not happy with the result, further corrective or revision surgery has significantly increased risks of complications whereas a pectus implant would be a safer option.
The implant is a solid but flexible and soft elastomer made from high quality medical grade silicone, supplied by NuSil, an FDA-approved world leader in medical silicone. The implant is made by Sebbin who have been manufacturing silicone implants for over 30 years. The implant is in place for life and unlike a breast implant, it is a solid block of silicone rather than a gel-filled envelope. This means it is unbreakable, will not rupture and there is no risk of leakage due to the solid construction. There are no issues with post-operative capsular contracture which is the most important complication of silicone breast implants.
The use of prosthetic implants for treating pectus excavatum has been used for many years with increasing improvements in material composition and tissue compatibility of the chest silastic elastomers used. More recently, the use of 3D printing technology has allowed the manufacturer of custom fitted implants that are based on precise CT or scanner measurements of the chest deformity. Though not widely available, it has an established role in treating adults with psychological concerns and offers a predictable result with a minor procedure.
The 3D custom pectus implant created by AnatomikModelling and the surgical approach used was developed by Prof Chavoin, a leading French surgeon and his team. The Pectus Clinic was the first surgical group to bring the 3D pectus implant and Prof Chavoins technique to the UK. We would be happy to share our experiences and results.
Ideally yes but it is not essential. Sometimes apparent funnel chest may be caused by another issue, or be associated with other problems. In that regard seeing your GP for an initial assessment and appropriate tests before seeing the Pectus Clinic may be helpful. Remember the Pectus Clinic is run by doctors and it is regarded as good practice that the Pectus Clinic receives a referral from your GP and it will assist in booking the appointment at Spire St. Anthonys Hospital. Following the consultation, a clinic letter (unless otherwise requested not to) will be sent to your GP and/or referring doctor.
Yes. You will require a Chest CT scan to allow detailed measurements to be taken of your chest wall deformity. It will also help the Pectus Clinic decide what is the best treatment option for you. In addition, depending on symptoms the Pectus Clinic may require further investigations to clarify if you have any ‘functional’ issues particularly with your heart and lungs. The chest CT scan can be arranged through a Spire hospital.
Following the consultation, a Chest CT is required and will help the surgeon choose the best option for you. If that is a pectus implant, working closely with Anatomik Modelling, pioneers in this technology, a 3D reconstruction from your scan is created allowing a precise assessment of your pectus excavatum to be made. Following this design process and review by the surgeon, the measurements and design are passed on to Sebbin, a company specialising in implant manufacture to create the custom implant that will fit your deformity precisely.
The process from CT scan to design and finally manufacture takes approximately 8 weeks and needs to be considered prior to agreeing on your date for surgery.
Under general anaesthetic, a small midline incision is made in the centre of the chest and taken toward the breast bone. The chest muscle is then expertly lifted off the breast bone and rib cage creating a precise platform for the custom fitted implant to be inserted fitting the pectus deformity like a glove. By placing the implant deep to the muscles, it provides a very natural correction of the chest and avoids the implant being visible below the skin particularly when moving, a criticism of other more superficially inserted non-custom implants performed by non-specialist cosmetic and plastic surgeons.
Yes, probably. A small drain or tube is usually placed at the end of the operation under the skin in the soft tissues to allow any fluid that builds up after the surgery to be drained.
Typically, you will be hospital just 1 night and rarely 2 nights following surgery. If a drain is used, patients are discharged with the drain in and advice about wound and drain management before discharge will be given. The drain is attached to a small bottle that can be worn on a belt or sling under clothing. After discharge, we recommend a short period of usually 5-10 days off work or college depending on how physical that work is. Most patients take simple over the counter painkillers during this period only. Further advice will be given if you have specific issues such as a very physical job.
Overall the recovery period is approximately 4-6 weeks, during which time you should be able to do normal activities and return to work/college. Sport should be best avoided in that first 4-week period. Light or aerobic exercise is generally OK after that but how much and what type will be discussed with you in your follow-ups appointments. If weight training is a big part of your life we recommend avoiding heavy chest type lifting exercises (such as bench presses) for up 12 weeks as the chest muscles need time to heal.
Following the operation, you will need to wear a compressive support for an approximately 4 weeks to help the swelling and oedema after the operation settle. For the first week or two, the support is like a corset and is worn every day and taken off for short periods only. After that we switch it to compressive vest for the final 2-3 weeks. The supports help the local swelling and oedema following the surgery settle. One of the side effects of the surgery is seroma (fluid) formation around the implant.
Following the operation, you will need to be seen within the first week of discharge. This is to assess your recovery, the degree of swelling and oedema and specially to look for seroma or fluid built up around the implant and how much fluid is draining. Seroma happens in all patients and is normal. The drain that you probably have been discharged with will deal with the seroma. If no drain was used the seroma feels like ‘bogginess’ under the skin. This will need to be aspirated or removal. Typically, seromas occur for the first few weeks and means you need to be seen once a week for an assessment and if no drain was used for the fluid to be removed. The drain if used is normally removed 1-2 weeks following surgery.
Serous fluid or seroma temporarily builds up around the implant immediately after the surgery and requires draining. if a drain was not used, this involves painlessly aspirating or removing the fluid in the outpatient clinic with a needle. Typically, this needs to be repeated each week after the surgery.
Yes, often and for most patients, the fluid build-up or seroma after the surgery is managed using a small drain tube inserted during the operation. You will be discharged with the drain in and showed how to look after it. This stays in for several weeks and allows the fluid to drain passively and is removed once fluid drainage is acceptable. You would still need to be seen regularly.
The surgery is minor and if you are otherwise fit and well the risk from the general anaesthetic or operation causing a serious or potentially life-threatening complication is very low. However, complications do occur and may require additional follow-ups, treatments including dressings, antibiotics, drainage or even further surgery.
Complications associated with this type of surgery include:
- Serous effusion/seroma – this is not regarded as a complication as it occurs in all patients and requires draining following the surgery.
- Skin bruising/Swelling – occurs after following all surgery. Bruising last 2-3 weeks but swelling can persist for many months.
- Numbness/sensitivity/discomfort – anaesthesia of the skin around the wound and in the chest is normal but typically regresses spontaneously over a few months, though a small area of permanent numbness may persist around the scar.
- Scarring – Since the healing process involves a somewhat random phenomenon, sometimes scars are not, in the end, as discreet as desired, and might have very different aspects: wide, retractile, adhesive, hyper or hypo-pigmented, hypertrophic (swollen) or even exceptionally keloid.
- Haematoma – or bleeding is a risk after all surgery and in this operation, would result in a haematoma around the implant that may develop in the first hours after surgery and may require a return to theatre to evacuate the blood. It is rare and generally avoidable with meticulous haemostatic precautions. Occasionally, a haematoma can develop later (what is called a secondary haematoma) and may be caused by excessive trauma or premature physical activity. It may be possible to manage with simple drainage but may also ultimately need further surgery to evacuate.
- Wound healing problems – associated with the scar can occur including wound dehiscence where the wound opens partly or even completely. It usually caused by excessive movement or tension and may be associated with premature physical activity or persistent coughing.
- Infection – Rare and all precautions including antibiotics during and immediately after surgery are given to reduce the risk. In rare occasions, if the implant become infected it will need to be removed.
- Malposition/displacement/movement of the implant – Due to its deep position, technique of insertion and custom fitting this is a rare long-term complication.
Unlike soft silicone gel breast implants the more solid pectus implants do not fold; are not associated with capsular retraction and cannot rupture and so are designed to be retained for the rest of the patients life.
Due to the specialised nature of the Pectus Clinic a combination of partial corrective surgery and pectus implants can be applied to achieve the best cosmetic results. In addition, working with experienced cosmetic plastic surgeons the pectus implant can be combined with breast augmentation for women with significant breast asymmetry (one breast much smaller than other) though it is advisable that the pectus implant and breast implants are performed at separate operations with a period in between to allow healing. This can be discussed in more detail at your consultation.
Gallery
We take numerous measurements and photos before, during and after Pectus Implant treatment as many of the problems we see centre around appearance. With the patient's permission we are happy to share our outcomes.
Results
It is important that we can show evidence that the Pectus Implant treatment we offer and the results that we achieve are proven. We actively collect data to allow us to study, research and publish are outcomes.
Please click on the buttons below to see and read about patients verified experiences (in their own words) and testimonials (which generally include before and after treatment photos). The pectus clinic is very grateful to all the patients who provided feedback.
