Nuss Procedure
Since the first report by Dr Donald Nuss in 1987 and the subsequent establishment of the procedure to treat pectus excavatum, there have many minor modifications to the Minimally Invasive Repair of Pectus Excavatum (MIRPE) technique. However, fundamentally it remains unchanged, that of placement of an internal ‘brace or bar’ to lift the sternum without removing or cutting of the cartilage or cutting of the breastbone.
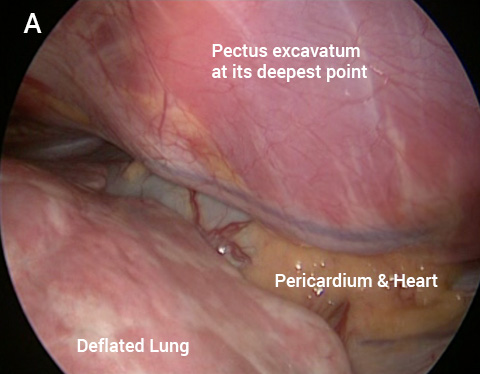
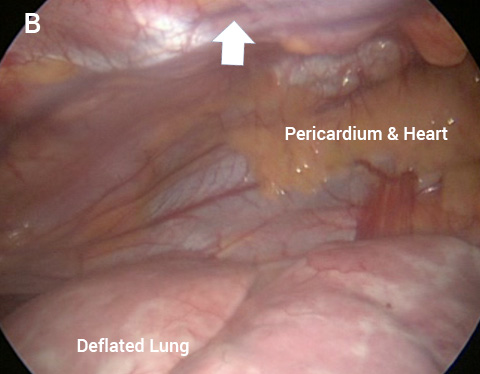
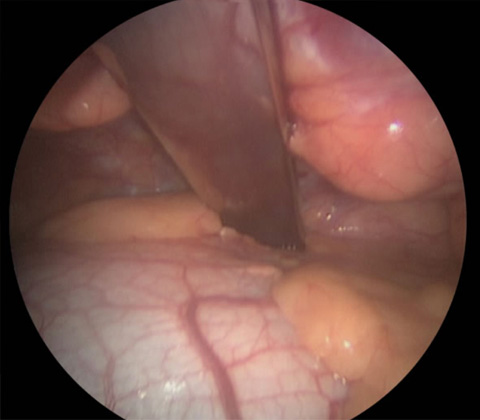
The keyhole image looking across the chest toward the heart and pericardium (heart sac) (A) before and following lifting the sternum (arrow) in a severe PE (B).
The MIRPE procedure is carried out as a minimally invasive or keyhole operation. With the patient on their back, two small incisions are made on either side of the chest wall. A telescopic video camera is placed into the chest through one of the incisions. The right lung is collapsed down to allow the surgeon to see across the chest using C02.
Please click on the buttons below to see and read about patients verified experiences (in their own words) and testimonials (which generally include before and after treatment photos). The pectus clinic is very grateful to all the patients who provided feedback.
This is followed by the careful insertion of one or two (rarely three) curved metal bars under the breastbone, the bar is then fixed in place. Occasionally to aid safe positioning of the bar, the sternum is lifted during insertion through a small 3rd incision made a the front of the chest. Once the bar/s are in place, It immediately corrects the pectus excavatum. They are not visible from the outside.
A drain is very occasionally left in the chest cavity to drain air or fluid at the end of the operation. The right lung is then re-expanded.
Following the operation (see video) which take anywhere between 1 to 3 hours a chest x-ray is performed to confirm position of the bar and lungs are fully re-inflated.
Click here to view the Nuss Procedure video
Warning: contains images of surgery. Must be over 18.
The video of the operation performed at St. George’s hospital was recently presented at the Society of Cardiothoracic Surgeons meeting in Glasgow and received the national best trainee presentation award
The bar is positioned in relation to the deepest point and immediately corrects the pectus excavatum
The immediate recovery time in the hospital is 3-5 days. Attention is paid to post operative pain relief and advice on how to move about to maintain the position of the bar.
After discharge, the patient is expected to slowly resume normal but restricted activity, such as heavy lifting or strenuous exercise. Follow up is typically at two weeks and then again at three to six months after surgery and then annually prior to removing the bar.
Increasingly the importance of physical therapy following surgery is recognised to both help the recovery and to improve on some of the typical issues around poor posture and muscle tone common in pectus excavatum patients. Often ’re-training’ the breathing muscles and encouraging deep breathing is also encouraged.
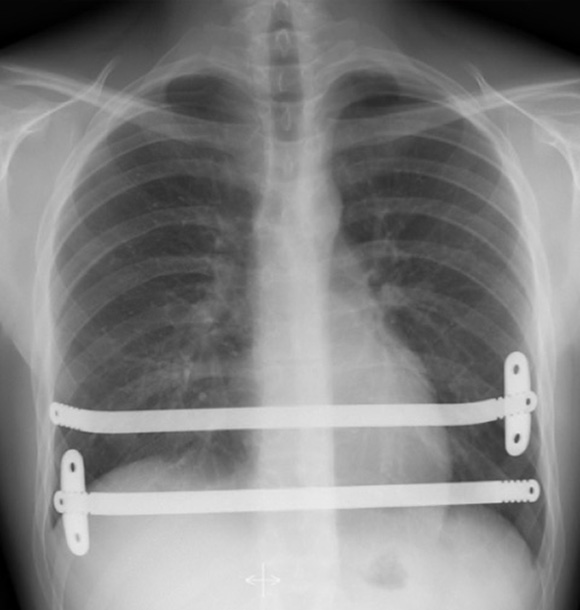

Post-operative Chest X-ray’s showing a 2-bar technique with one stabiliser on each bar (Left) and 1-bar with two stabilisers (Right). Note significant spinal scoliosis or sideways spinal curvature


Pre (left) and post (right) Nuss procedure in a 16 year old

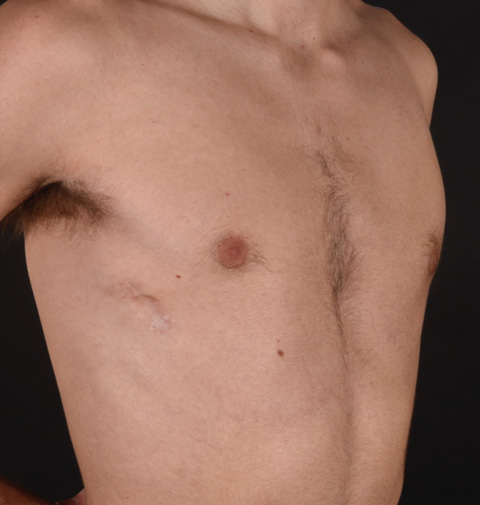
Pre (left) and post (right) Nuss procedure in a 32 year old
The pectus support bar is removed after between 2-3 years. It involves a short general anaesthetic and can be performed as a day case procedure with resumption to normal activities within a few days.
Examples of female corrective Pectus Excavatum Surgery
Frequently Asked Questions about the Nuss or MIRPE procedure for treatment of pectus excavatum
Named after the first surgeon who described it, Dr Donald Nuss, it is an invasive corrective keyhole operation to insert an internal metal bar/s to brace or push the breastbone forward. MIRPE stands for Minimally invasive repair of pectus excavatum and is used as an alternative name to the Nuss operation. The surgery aims to permanently correct the pectus excavatum and return the chest to a normal or near normal position.
The procedure is carried out under General Anaesthetic (GA, asleep) as a minimally invasive or keyhole operation. The operation takes around 2-3 hours to perform. Two small incisions are made on either side of the chest wall with a camera placed into the chest through one of the incisions. This is followed by the careful insertion of one or two (rarely three) curved metal bars under the breastbone, the bar is then fixed in place. Sometimes to aid safe positioning of the bar, the sternum is lifted during insertion through a small 3rd incision made at the front of the chest. It immediately corrects the pectus excavatum and is not visible from the outside. The wounds are closed with absorbable (internal) sutures (stitches) and covered with dressings.
For most patients with pectus excavatum a Nuss operation is a good choice. However, occasionally to achieve the best results the surgeon may recommend an open or Modified Ravitch operation (named after the surgeon who first described technique). Alternatively, occasionally a non-corrective option, a pectus implant may be offered (see Pectus Implants).
The Nuss or MIRPE operation has been performed for over 30 years by surgeons around the world and though there has been modifications of the original technique it provides a good way to push the breastbone forward to surgically correct the pectus excavatum with many scientific papers published supporting its use.
Mr Hunt, the Medical director of the Pectus Clinic is an experienced thoracic surgeon and has performed the Nuss or MIRPE operation since 2009 and has one of the largest Pectus surgical practices in the UK. We would be happy to share our experiences and results.
Ideally yes but it is not essential. Sometimes apparent funnel (dipped in) chests may be caused by another issue or be associated with other problems. In that regard seeing your GP for an initial assessment and appropriate tests before seeing the Pectus Clinic may be helpful. Remember the Pectus Clinic is run by doctors and it is regarded as good practice that the Pectus Clinic receives a referral from your GP and it will assist in booking the appointment at Spire St. Anthony’s Hospital. Following the consultation, a clinic letter (unless otherwise requested not to) will be sent to your GP and/or referring doctor. Note if using private health insurance, some insurers require a GP referral letter to a specialist prior to authorizing the consultation. If unsure, speak to your insurer.
Yes, for most patients. You will require a Chest CT or MRI scan to allow detailed assessments to be taken of your chest wall deformity. It will also help the Pectus Clinic decide what is the best treatment option for you. In addition, depending on symptoms the Pectus Clinic may require further investigations to clarify if you have any functional issues particularly with your heart and lungs such as an Echocardiogram.
Instructions on preparing for your admission will be provided by Spire St. Anthony’s hospital and you will have an opportunity to discuss the admission process with the pre-admission team before the day of surgery. Typically, a pre-assessment including blood tests is required. Details on when to stop eating and drinking and what time to come to hospital and what to bring will be provided by the Spire pre-assessment team. If you are taking certain medications that ‘thin’ the blood, such as aspirin or warfarin or certain painkillers such as Ibuprofen, we will discuss whether they will be needed to be stopped before the surgery.
Before: You will be admitted on the day of the operation and must fast (Nil by Mouth) before the operation. You will meet the nursing and physiotherapy team and an opportunity to discuss your stay in hospital, restrictions and exercises following surgery. You will meet the anaesthetist and discuss the general anaesthetic and particularly pain control after the operation. You may be offered a spinal injection, which acts to help reduce pre-emptively the pain following the surgery.
During: Making small incisions and using local anaesthetic nerve blocks will help reduce the pain after the operation. With the increasingly common use of intra-operative cryotherapy the need for very strong painkillers [opiates] after the operation has been reduced. Cryotherapy ‘numbs’ the chest and reduces pain, The numbness may last for weeks and occasionally months.
After: You will be transferred to the recovery area and a chest x-ray will be performed to confirm the lungs are fully re-expanded. You will be transferred to the ward or the high dependent unit following the surgery. You will be offered a Patient Controlled Analgesia or PCA pain pump following the surgery. This is a drip which allows you to administer painkiller directly in which you can control based on your pain experience.
You will be in hospital typically 3 days. A drain/s may be put in at the time of the operation to drain any blood or air that collects after the surgery. This will be removed. Antibiotics will be administrated to reduce the risk of infection and treatment to prevent blood clots (TED stockings and blood thinning medications) until you are walking. You will be encouraged to walk the next day and with the help of physiotherapy breathing exercises will be started.
Physical activity: It’s important that the day following the surgery you begin to mobilise, and you will be encouraged to sit out of bed, start walking and begin physiotherapy exercises. It helps reduce risks of blood clot and chest infections. It helps your bowels begin to work and start to feel like eating again.
Pain control: You will have a chance to discuss pain control before the surgery with the anaesthetist. The spinal injection if given before the operation helps pain control in the first and second day after surgery but begins to wear off. Cryotherapy if used during the surgery will help reduce the pain following the operation. The PCA is the main painkiller used after surgery in the first day or two. In addition, regular analgesic tablets will be started. Pain is to be expected but should be acceptable and controllable. It’s important that you let us know if you are in pain, so we can tailor your pain control to your needs.
Constitutional symptoms: Your bowel habit and appetite may be affected following the surgery and sometimes a laxative may be needed. We do not routinely use a urinary catheter but occasionally passing urine in the first few days after surgery can be difficult.
Dressings and washing: You will usually be able to shower within 24-48 hours after surgery. Dressings for the wounds will be managed by the nursing team and you will be discharged with dressings advice. If a drain was used, advice will be given about dressings.
We will plan your discharge with you, your family and the nursing and physiotherapy team. There are some restrictions of physical activity and that will be discussed with you in detail. Basically, you need to walk as much as you can and continue the physiotherapy breathing exercises including incentive spirometry (a machine that you breath into that encourages you to breathe deeply). A discharge plan will be discussed with you including wound dressings and painkillers to take. If a drain/s were used a drain stitch (suture) will need to be removed by your general practice about 7 days after discharge.
Every patient is different but on average it takes about 4 to 6 weeks to recover from the surgery though it will take up to 12 weeks before you return to full and normal physical activities including sports and exercise particularly if the patient experiences a complication such as a wound infection. Returning to work/studies is variable and depends on what type of work you do but on average is around 4-6 weeks.
Following discharge, you will be given advice about what to expect in the coming days and weeks after the surgery.
Pain after surgery: It is normal to have some pain in the chest after the surgery and you will be given several different oral painkillers including strong painkillers to take regularly. Over the coming weeks the stronger painkillers can be reduced and replaced with Over the Counter (OTC) painkillers such as Paracetamol or Ibuprofen taken for as long as you feel the need to. Most patients take painkillers regularly for the first 4-6 weeks.
Wounds: Your surgical scars, typically 2 with one on each side of the chest and occasionally a third small incision at the front of the chest will be covered with dressings and advice will be given prior to discharge. The dressings are kept for about a week and then removed around 7 to 10 days after discharge. There should be no stiches to remove unless you have had a drain/s. The wounds may be a little swollen and bruised in the first few weeks. You can shower during this time, though try and keep the wounds dry (covering the wound with clingfilm when in the shower can help).
Constitutional symptoms: It’s quite common in the few weeks following surgery to feel ‘off your food’, feel tired and have changes in your bowel habit (constipation). Many patients report losing weight following the surgery. It’s important that your recover ‘well’ after the operation, so eating well, regular activity (walking) and a return to normal daily activities (not exercise) is encouraged in the first 4 weeks after surgery.
First 4-6 weeks: To avoid excessive pain and to reduce the risk of the bar/s used to correct your pectus from moving or becoming dislodged. This includes:
- Sleeping on your back and avoiding sleeping on your side
- Avoid sudden and excessive bending or twisting your upper body
- Avoid lifting / carrying heavy weights that require you to strain
- Walking and deep breathing exercises are encouraged
Next 6 weeks: Increase your level of physical activity including aerobic activities such as jogging, cycling and swimming. You are able to lift / carry more weight but continue to avoid weight lifting.
After 12 weeks: You are able to return to all physical activity and sports however, if you participate in potentially violent contact sports such as rugby or martial arts some caution is required, and further advice can be offered if these sports are important to you. The chest may continue to feel numb if cryotherapy was used at the time of the operation.
The bar is unlikely to cause the metal detector to alarm. You will be offered a card to carry. Alternatively, carry a clinical letter.
The surgery is invasive but if you are otherwise fit and well the risk from the general anaesthetic or operation causing a serious or potentially life-threatening complication is very low. It is important to be aware that though only rarely reported in the medical literature there have been cases of heart injury resulting in death.
Complications associated with this type of surgery include:
- Bleeding - is uncommon occurring 1-5% of cases and can occur during or after the procedure. At the time of the surgery, it can usually be stopped simply but may require a bigger cut to be made. After surgery, bleeding can occur and result in a haemothorax (blood in the pleural cavity) which may require a chest drain to be inserted or return to theatre to evacuate the blood.
- Pneumothorax occurs when the lung following surgery does not fully re-expand and air in the pleural space remains. In most cases it can be monitored following surgery with chest x-rays and in less than 1% of cases requires a chest drain to remove the air.
- Pleural effusion is fluid building up in the pleural cavity around the lung. Despite being rare, it can be monitored with chest x-rays and in less than 1% of cases requires a chest drain to remove the fluid.
- Pericarditis / Pericardial effusion is thought to be caused by inflammation of the lining of the sac of the heart with rare fluid built up around the heart. It is rare but unpredictable and is usually treated with rest and anti-inflammatory medication. The pericardial effusion may need to be monitored and very rarely drained.
- Wound Problems including:
- Infection – All precautions including antibiotics during and immediately after surgery are taken but wound infection is a risk with all surgery. If infection occurs, dressings and antibiotics are usually all that is required. Rarely, further surgery to clean the wound is required.
- Seroma – Build-up of a fluid in the wound, is uncommon but can occur even several weeks after surgery. Simple compressive dressings are all that is usually required.
- Numbness – anaesthesia of the skin around the wound is normal but typically regresses spontaneously over a few months, though a small area of permanent numbness may persist around the scar. Use of cryotherapy may aggravate the sensation of numbness across the chest.
- Healing abnormalities – Since the healing process involves a somewhat random phenomenon, sometimes scars are not, in the end, as discreet as desired, and might have very different aspects: wide, retractile, adhesive, hyper or hypo-pigmented (darker or lighter scars), hypertrophic (swollen) or even exceptionally keloid (The name given to a scar that overgrows and becomes larger than the original wound).
- Chronic wound issues – following a wound infection or seroma the wound can become chronically inflamed requiring occasional use of dressings, aspiration (fluid removal) and antibiotics. If persistent there is a risk that the bar will need to be removed.
- Displacement/movement of the bar can occur following the operation. With modern modifications to the bar insertion, the risk is low at around 2% though historically was more common. The risk of bar displacement is typically in the first 6 weeks and can be reduced by restricting physical activities during this period. Advice will be given but sudden twisting movements particularly when lifting should be avoided. If you have sudden severe pain and feel bar movement, you must let us know.
- Chronic Pain associated with the bar after surgery has been described and is usually mild, intermittent and can be related to specific movements or activities. It is not common, rarely significant and can be treated with painkillers if needed.
- Bar felt/seen – in very slim patients the bar may be felt or rarely even seen, particularly with certain movements.
Following surgery arrangements will be made for a follow-up appointment usually around 4 weeks following discharge and then once again at around 12 weeks after surgery. After that we would recommend an annual review until the bar is removed. Following the 4-week follow-up most patients able to consider significant travel commitments including air travel. By the 12-week (3 month) follow-up most patients ‘back to normal’ with no restrictions on activities.
We do recommend the bar is removed and not simply left in as once the chest wall has corrected and remodelled as the bar serves no ongoing purpose. Typically, the bar is left in for 3-4 years and then removal is offered.
Removing the bar involves a general anaesthetic through the same incisions the bar is removed. It is typically done with a one-night stay. Very occasionally a soft tissue drain may be used in the wound though this is uncommon. The operation is regarded as minor, however there have been reports in the literature of bleeding complications when the bar is removed including rare deaths reported worldwide. Therefore, specific precautions including equipment to enlarge the incision are made available. In addition, sometimes the bar can be difficult to remove due to ‘overgrowth’ of bone around the bar requiring surgery to free the bar prior to removal. Recovery is usually just a few days on painkillers and return to work/college around 1-2 weeks following surgery.
Often a concern, the risk of relapse particularly significant relapse is low (<2%) and may be related to the bar being removed prematurely or in young patients a late (post bar removal) further growth spurt.
Please click on the buttons below to see and read about patients verified experiences (in their own words) and testimonials (which generally include before and after treatment photos). The pectus clinic is very grateful to all the patients who provided feedback.