Pectus Excavatum
The most common chest wall deformity, pectus excavatum or sunken chest is most likely caused by abnormal growth of the costal cartilage junction between the ribs and sternum. It can present in toddlers but typically becomes apparent during the growth spurt and puberty.
Amongst doctors dealing with pectus excavatum there is a lot of discussion around whether pectus excavatum can cause significant symptoms and signs. Symptoms are what patients complain of, whether as signs refers to objective evidence of disease as observed by a health care professional.
Please click on the buttons below to see and read about patients verified experiences (in their own words) and testimonials (which generally include before and after treatment photos). The pectus clinic is very grateful to all the patients who provided feedback.
Symptoms
The presence of symptoms in patients with pectus excavatum is variable. Certainty chest and back pain is common and is probably musculoskeletal in origin. Another common complaint is the sensation of breathlessness, particularly on exertion. Poor posture, which is often present maybe a factor in the development of such pain and breathlessness. The psychological impact of the abnormal chest appearance is probably the most important symptom that patients with pectus excavatum complain of. In some, it can have serious consequences leading to withdrawn behavior, avoidance of certain activities like swimming or places such as the beach where the chest may be exposed and the development of intimate relationships often at and important and vulnerable time of the patient's life. Rarely, in severe forms of pectus excavatum patients' doing vigorous exercise may complain of feeling faint or actually fainting.
Signs
Most doctors recognize an apparent association between the sunken appearance of the chest and reduction or restriction in lung function as well as physical displacement of the heart causing symptoms such as breathlessness. However, when measured lung or pulmonary function at least on simple testing (spirometry) appears usually normal in most patients with pectus excavatum. But measured with more sophisticated tests particularly involving measuring when exercising (cardiopulmonary exercise tests) studies have demonstrated a relationship between experience of breathlessness on exertion and a reduction in pulmonary reserve. Following surgical correction studies have demonstrated in severe forms of pectus excavatum pulmonary reserve and exercise tolerance is improved, however this finding is not universal across all studies.
In pectus excavatum the sternum is pushed backwards and the heart which sits behind and slightly to the left of the the sternum can be displaced and may affect cardiac function in severe forms. Again though not universal, some studies have found surgery to correct pectus excavatum can improve cardiac function when carefully measured.
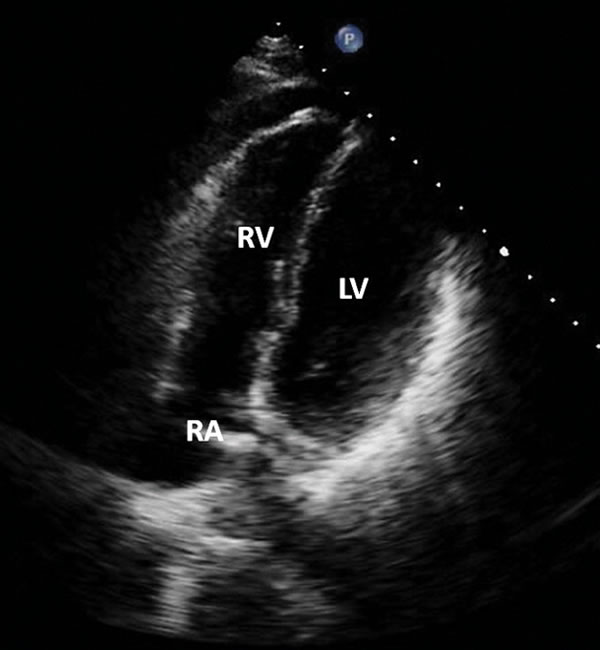
Echocardiogram of heart
Diagnosis
The diagnosis of pectus excavatum is what doctors call a clinical one, that is careful physical examination with a doctor familiar with pectus deformities is usually all that is required. There is no specific blood test, but radiological assessment (x-rays) may help assess the severity of the pectus excavatum and identify other associated problems such as scoliosis of the spine. The most useful radiological test is a Chest CT scan which allows a more sensitive assessment of the pectus excavatum particularly its severity and displacement of the heart, as well as degree of sternal rotation caused by asymmetry of the pectus. This is particularly important when planning type of surgery (NUSS vs. Open correction). MRI is an excellent alternative investigation that avoids radiation particularly in children.
Other investigations such as echocardiography (ultrasound assessment of the heart), and lung function testing are not necessarily required unless symptoms are severe and/or an underlying cause such as Marfan's syndrome is suspected.
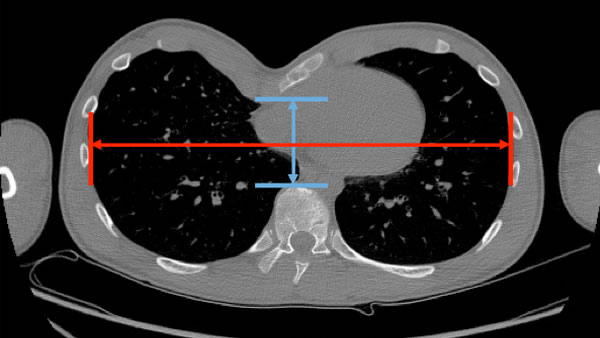
Chest CT scan showing the Haller index used to assess severity of the pectus excavatum, the blue line is called the anteroposterior (AP) distance and represents how close the back of the sternum gets to the front of the spinal or vertebral column. This distance is used to visually assess severity of the pectus deformity. When calculated as a ratio against the red line, the transverse chest wall distance, the greater the ratio the more severe the pectus excavatum.
Chest CT scan showing a young man with a moderate severe asymmetrical pectus excavatum deformity. Note the clinical distance or depth of the pectus; how the heart is pushed over to the left and is indented by the sternum which is also rotated or tilted.
Severity
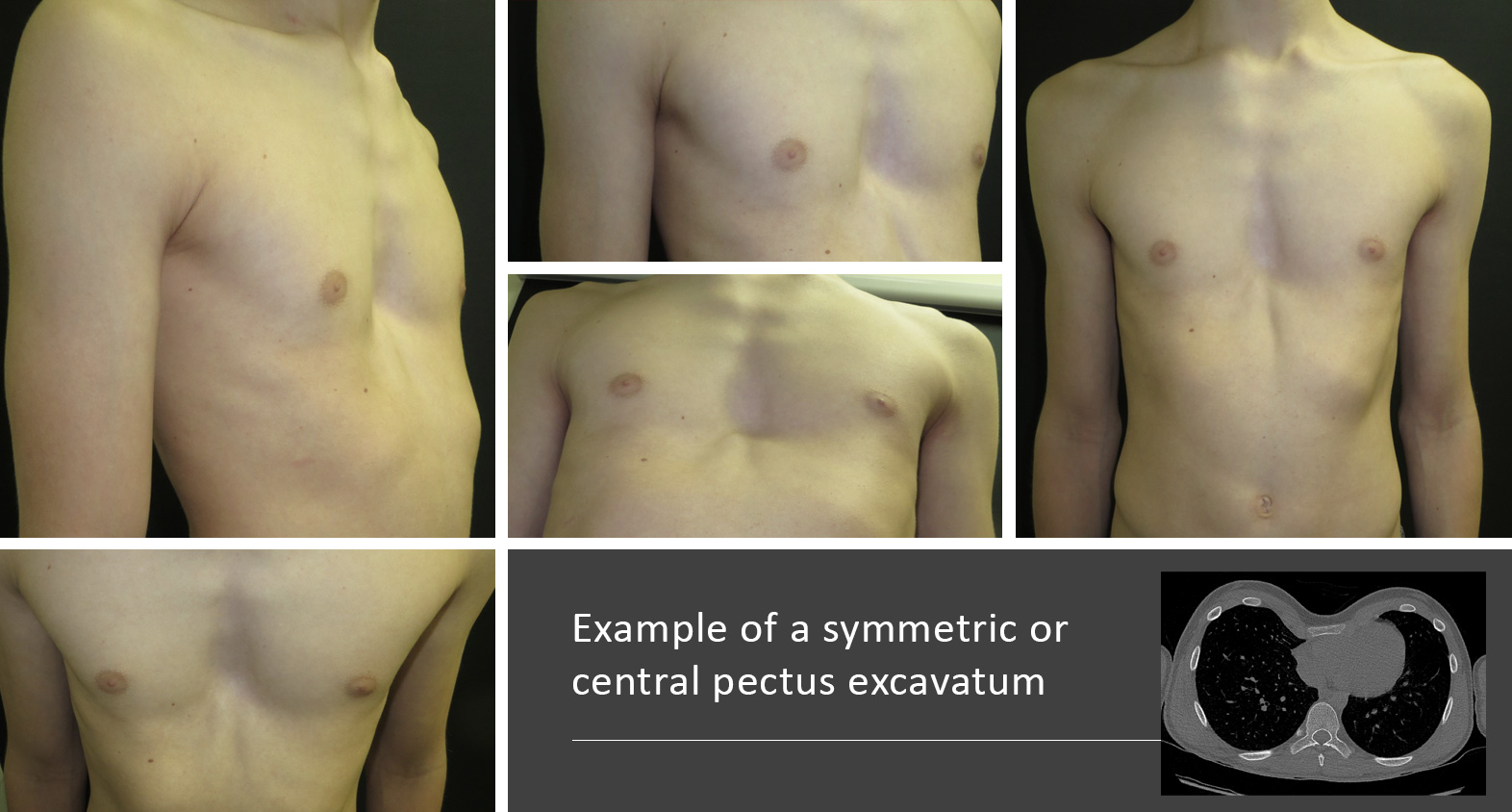
The is quite a lot of variation in severity (generally regarded as the depth the sternum is pushed back toward the spinal column) with the lower part of the sternum usually more affected. Degree of asymmetry between the right and left sides of the chest causing the sternum to rotate as well as other associated musculoskeletal effects including compensatory rib flaring (where the lower rib cage sticks out) and less commonly rib flattening adds to the severity of the deformity. Poor posture often accompanies pectus excavatum with shoulders slumped forward and the upper spine curved forwards, as well as other spinal problems such as scoliosis.
Simple clinical description of severity of pectus is based on the depth the sternum is pushed inwards. Other ways of describing pectus excavatum include the type of deformity such as 'trench-like', cup-shaped or saucer-shaped.

Mild symmetrical Pectus excavatum with a cup shaped deformity and minimal rib flaring

Moderate symmetrical pectus excavatum with more of a saucer shaped deformity and minimal rib flaring

Moderate symmetrical pectus excavatum with more of a cup shaped discrete deformity and moderate rib flaring

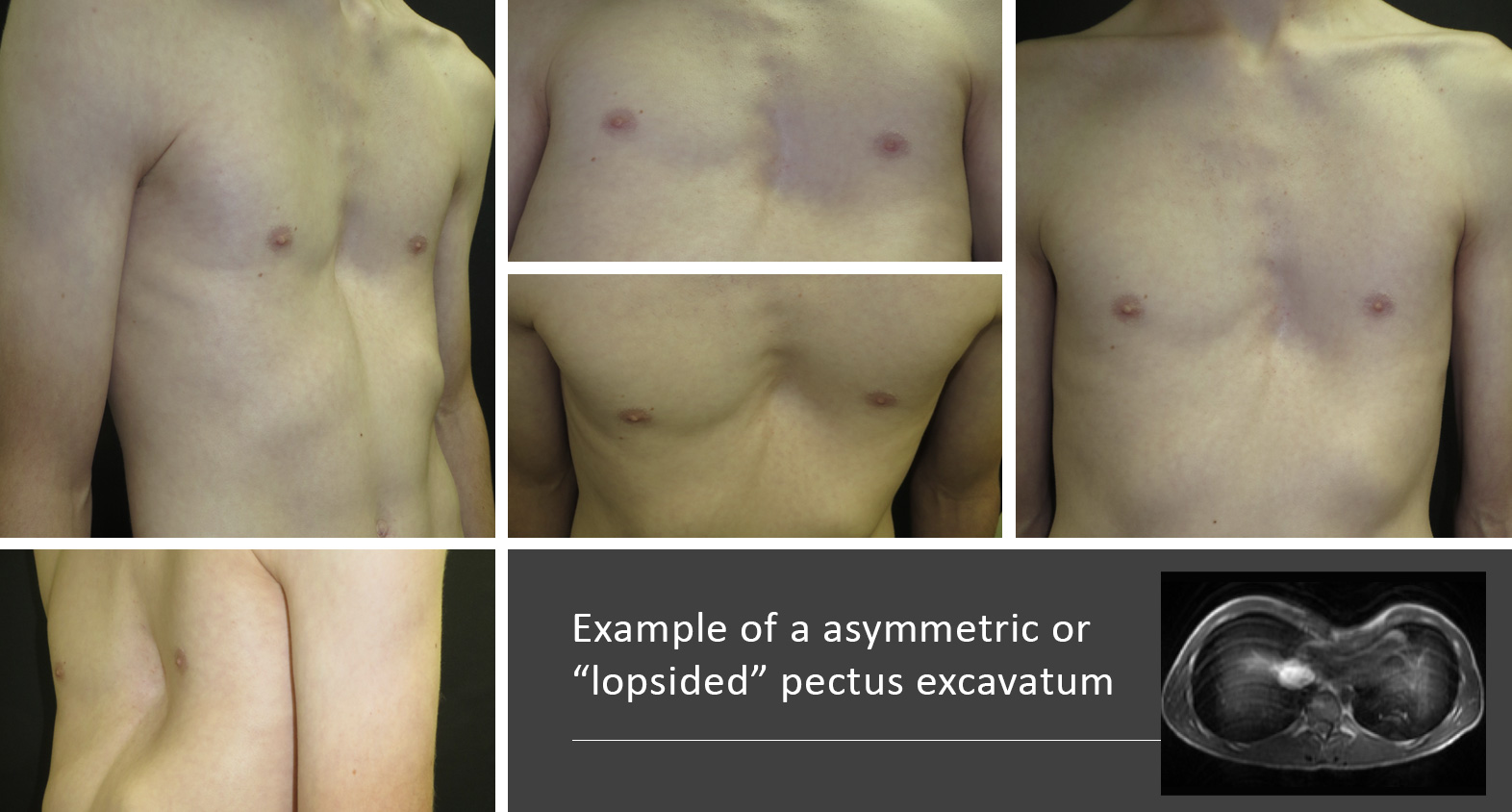
Severe asymmetric Pectus excavatum with a broad deformity and moderate rib flaring

Severe asymmetric pectus excavatum with a trench like deformity and some rib flattening
Simple clinical description of severity of pectus is based on the depth the sternum is pushed inwards. Other ways of describing pectus excavatum include the type of deformity such as 'trench-like', cup-shaped or saucer-shaped.
In females with Pectus excavatum consideration of breast asymmetry, size variation or abnormality must be factored into any treatment plan as it may be affect the final outcome.
Examples of female corrective Pectus Excavatum surgery
Gallery
We take numerous measurements and photos before, during and after vacuum bell or surgical treatment as many of the problems we see centre around appearance. With the patient's permission we are happy to share our outcomes.
Results
It is important that we can show evidence that vacuum bell or surgical treatment we offer and the results that we achieve are proven. We actively collect data to allow us to study, research and publish are outcomes.
Please click on the buttons below to see and read about patients verified experiences (in their own words) and testimonials (which generally include before and after treatment photos). The pectus clinic is very grateful to all the patients who provided feedback.