Vacuum Bell Therapy
The vacuum bell device was developed in 2005 by Eckart Klobe, over a decade ago and though not used regularly outside certain centres its has as gained a lot of publicity due to the fact it offers one of the only truly non-surgical treatments for pectus excavatum. Amongst doctors treating pectus excavatum the vacuum bell is increasingly being used as a way of lifting the breastbone temporarily during the NUSS procedure to allow the bar to be safely inserted behind the breastbone. Otherwise, there are some reports of good results in young patients with pliable anterior chest walls though long-term results and application in older patients remains less clear.
After an initial consultation we will assess the most appropriate treatment method for your pectus deformity. Whether it be invasive or non-invasive, we ensure your treatment will be of the highest quality, tailored to your individual needs. Following a 3D scan, If the vacuum bell is considered an option careful measurement and positioning of the vacuum bell over the pectus and then application of suction to bring the sternum forward will be undertaken as part of the assessment. It is worn several hours each day over 6-12 months in patients with pliable pectus excavatum. However, the long term results are still undergoing medical assessment.

Types of Klobe Vacuum Bell: the pectus clinic works with Eckart Klobe, the inventor and manufacturer of the Klobe Vacuum bell, the first device developed specifically to offer a non-surgical treatment for pectus excavatum (photo provided by Eckart Klobe).
Please click on the buttons below to see and read about patients verified experiences (in their own words) and testimonials (which generally include before and after treatment photos). The pectus clinic is very grateful to all the patients who provided feedback.
 Pectus Excavatum in a teenage boy before starting VBT
Pectus Excavatum in a teenage boy before starting VBT
 After VBT for approximately 1 year wearing the VB every evening
After VBT for approximately 1 year wearing the VB every evening


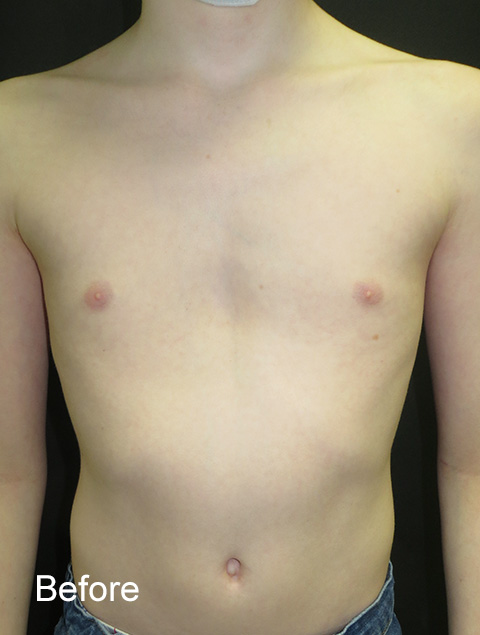

Before and after images shown using the slider (drag central cursor left or right to view) of two patients with pectus excavatum before and around 12 months of VBT treatment.
Frequently Asked Questions regarding Vacuum Bell therapy for treatment of Pectus Excavatum (Sunken Chest)
The Vacuum Bell was developed by Eckart Klobe in 2002 and is the only non-surgical treatment for sunken or funnel chest (Pectus Excavatum). It works by lifting the breastbone and front of the ribcage by creating a partial vacuum. It relies on some ‘flexibility’ of the chest as well as time for chest wall remodelling and correction to take place, and so requires a period of sustained wear to create an improvement in the pectus deformity.
Treatment with VBT is NOT established within any current recommendations or guidelines but remains a popular non-surgical option in treating flexible Pectus Excavatum as the alternatives are only surgical (corrective surgery such as the Nuss procedure or non-corrective surgery such as a pectus implant).
In the medical literature there is some evidence of the effectiveness of VBT and Mr Hunt has published a review of the current evidence. He concluded that:
"VBT is a safe therapy for treating pectus excavatum in a non-surgical conservative manner with few complications reported. However, the success of VBT is largely dependent on patient compliance and motivation. Permanence of correction after completion of VBT needs to be properly assessed through rigorous follow-up, and currently the success of correction, i.e. permanence, remains in the hands of the patient."
Yes. The Pectus Clinic is run by doctors who practice evidence-based practice and are ethically obliged to offer treatments that are likely to be successful. In that regard, data is collected and outcomes of patients who have been treated with VBT by the Pectus Clinic have been published in peer reviewed journals and presented in national and international meetings. However, its long-term outcomes (years after treatment stopped) remains currently unproven.
The technique is aimed at treating patients, male or female with this type of deformity. However, the Pectus Clinic believes as with bracing for pigeon chest, there are three important considerations: Age; what is called ‘musculoskeletal maturity’ (essentially both reflect chest wall flexibility); and the type and severity of the pectus excavatum.
The Vacuum Bell works by lifting through a partial vacuum the breastbone and anterior chest wall and also stretches internal muscles including the diaphragm so overcoming the tendency of these muscles to pull the ribcage inwards.
Age is important and is a useful guide to how much flexibility the chest has. As we get older these cartilaginous joints become increasingly stiff and bone-like making correction more difficult. People ‘age’ at different rates and so even though they may be in their 20’s they still may have some flexibility in these joints and of course vice versa. This is what musculoskeletal maturity means.
Finally, most types of Pectus Excavatum tend to involve the lower breastbone and to be in the middle (symmetrical) of the chest. The depth of the funnel chest varies and typically is described as mild, moderate and severe. In addition, the shape of the pectus deformity varies and can be described variously as ‘cup-shaped’ (discrete), saucer shaped (flat) and grand canyon (trench-like). The shape and depth of the Pectus Excavatum along with body shape (slim, heavy, muscular etc.) may influence effectiveness of the Vacuum Bell and are all important considerations.
Mr Hunt, the Pectus Clinic Medical Director and a very experienced consultant Thoracic (chest) surgeon clinically assesses all patients prior to recommending VBT.
One reason is that you have been miss-diagnosed, and that you don’t have a Pectus Excavatum. Expert assessment by Mr Hunt prior to starting VBT ensures the correct diagnosis and the correct treatment offered.
In addition, other reasons (contraindications) to VBT include: Presence of skeletal disorders leading to ‘bony weakness’ such as Osteogenesis Imperfecta (brittle bone disease) and Osteoporosis (‘thin bones”); Angiopathy or disease of the great blood vessels (aorta) associated with Marfan syndrome or Aortic Dilation (Aneurysm); Coagulation disorder (bleeding disorder) such as haemophilia.
Though not a contraindication in patients who play violent or heavy contact sports particularly at as high level such as wrestling, or rugby caution is advised during the treatment as the chest wall during VBT may experience a temporary reduced firmness.
Rib flare where the bottom of the rib cage sticks out is common in both funnel and pigeon chest and with other types of pectus deformity. It is often quite prominent, particularly on the left and can occasionally become more obvious when treating funnel chest with VBT especially in young patients. In this situation, time and exercises are often all that’s needed to improve its appearance. However, sometimes we recommend using a custom fitted ‘rib strap’ designed by the Pectus Clinic to help support the rib cage during VBT. Occasionally, if the rib flare is severe, we may recommend a specially designed rib flare brace.
Ideally yes but it is not essential. Sometimes apparent ‘sunken-chest’ may be caused by another issue or be associated with other problems. In that regard seeing your GP for an initial assessment and appropriate tests before seeing the Pectus Clinic may be helpful. Remember the Pectus Clinic is run by doctors and it is regarded as ‘good practice’ that the Pectus Clinic receives a referral from your GP, and it will assist in booking the appointment at Spire St. Anthony’s Hospital. Following the consultation, a clinic letter (unless otherwise requested not to) will be sent to your GP and/or referring doctor.
Yes, generally. The Pectus Clinic will request photographs of your chest wall deformity and some basic medical information about your issue. If following this ‘screen’, the Pectus Clinic’s Medical director, Mr Hunt, will make arrangements to see you. The consultation will clarify the diagnosis of funnel-chest, the need for further investigation, concerns around suitability for the Vacuum Bell treatment or any other issue related to your pectus deformity.
Please contact the Pectus Clinic Administrator for a prompt reply and details including information required.
An initial consultation with Mr Hunt normally takes around 45 minutes and include clinical assessment, photographs, measurements to assess suitability of VBT and a 3D scan as well as discussion about what the treatment involves. A brief ‘trial’ of the Vacuum Bell to assess suitability and choice of which Vacuum Bell to offer is included.
No, generally not for VBT though if surgery for your Pectus Excavatum is being considered it may be recommended. Also, if there is doubt about the pectus diagnosis or the best treatment to recommend, a radiological investigation to assess further will be requested but this is not usual. Very occasionally, a further genetic assessment may be requested if there are concerns of an underlying congenital or genetic disorder such as Marfan syndrome.
Nothing specific but would suggest wearing loose fitting clothes and coming with a friend or relative. You will be fine to travel by public transport or drive home.
The Pectus Clinic provides detailed written information about wearing the Vacuum Bell, its maintenance and lots of useful tips as well as a detailed written customized wearing schedule which will be explained to you.
The wearing schedule is based on extensive analysis of the data collected by the Pectus Clinic and knowledge of other VBT programs around the world.
At the fitting appointment: The first application of the Vacuum Bell should be supervised by medical personnel. Whilst lying down the patient learns to position the Vacuum Bell and to apply it in a way which is snug and comfortable. The patient learns to use the pump to generate the vacuum. You may feel the pull of the Vacuum Bell, and even feel a little uncomfortable but it should not be painful. With the Vacuum Bell applied, the patient may stand up and walk around. Typically, the first application is for 10-15 minutes.
Progressively longer wearing: Over the first 4-8 weeks the Vacuum Bell is worn each day for increasing increments. A Suggested wearing schedule:
First Month
Wear the Vacuum Bell for up to 1 hour a day for the first 1-2 weeks (week 1-2)
Wear the Vacuum Bell for up to 2 hours a day for the next 2 weeks (week 3-4)
In this first month, most patients will see movement and lifting of the breastbone in response to the partial vacuum and the aim is to maintain this lift. Typically, younger patients will see such a correction in the first 2 weeks, with older patients (adults) seeing such a correction in the 3rd and 4th week.
Second Month
Wear the Vacuum Bell for up to 3-4 hours a day in the next 2 weeks (week 5-6)
Wear the Vacuum Bell for up to 4 hours a day in the following 2 weeks (week 7-8)
Third month and onwards
The aim is to maintain the chest correction by wearing the Vacuum Bell a minimal of 4 hours per day. If the Vacuum Bell can be worn more often if possible, there is some evidence that it will give a more consistent and possibly better outcome. It’s important to emphasize the most important element of the VBT is consistent daily wear, NOT increasing the suction particularly after the first few weeks.
There are few complications described during VBT if used appropriately but those described include:
On the first applications of VBT, dizziness if standing can occur and can be avoided by lying flat during the initial treatment.
Chest wall muscle ache is quite common and if persists or worsens a reduction in the partial vacuum or length worn may be required.
Backache can occur and may be related to alterations in posture and in response to changing chest shape. If persists or worsens a reduction in the partial vacuum or length worn may be required.
Gynaecomastia (or enlarged breast or nipples) particularly in older patients has been described and if occurs should be discussed with the Pectus Clinic as it may require changes to the VBT schedule.
Yes. Where the Vacuum touches the chest and specifically the skin over the pectus excavatum can be affected and care particularly in the first few weeks should be taken to avoid a skin problem.
Typically wearing the Vacuum Bell results in redness of the skin but this should only be temporary, and the redness should fade once the Vacuum Bell is removed. Advice will be given about what to watch for and how to look after your skin whilst wearing the Vacuum Bell.
If the partial vacuum is too strong or the Vacuum Bell is worn too long ‘petechiae’ (droplets of blood on the skin) can appear. Adjustment to length (shorter) worn and strength (reduced) of the Vacuum Bell should be made.
Bruising, with black or blue marks (haematoma) may develop if the Vacuum Bell is used for protracted periods and/or with excessive suction applied. Adjustment to length (shorter) worn and strength (reduced) of the Vacuum Bell should be made.
Over time and with protracted wear the overlying skin may become ‘flabby’. This is caused by a redistribution and accumulation of fluid in skin and soft tissues under the skin. Adjustment to length (shorter) worn and strength (reduced) of the Vacuum Bell should be made.
Skin abrasions can occur if the skin comes into contact with glass viewing panel of the Vacuum Bell for prolonged periods or by rubbing and movement of the Vacuum Bell lip on the skin surrounding the Pectus Excavatum. Adjustment to length (shorter) worn and strength (reduced) together with reducing physical activity whilst wearing the Vacuum Bell.
Irritated Nipples can occur particularly if the edge of the Vacuum Bell lies directly over the nipples and can remedied by altering position of the Vacuum Bell to avoid this. Alternatively, if this is not possible using nipple covers (plasters covering the nipples often used by runners to avoid ‘joggers nipple’ can be applied).
Change in skin sensation (slight numbness) can occur, particularly in the upper arms. Adjustment to length (shorter) worn and strength (reduced) of the Vacuum Bell should be made.
Please contact the Pectus Clinic if worrying complications occur, particularly if they persist following reduced Vacuum Bell wear, less suction or after the VBT terminated. Often sending a picture will help assessment.
The Vacuum Bell can be used during common daily activities including lying, sitting, standing, walking, running, whilst at school or at work. Non-contact sport activities can be continued whilst wearing the Vacuum Bell, but swimming and contact sports are generally not possible. Some patients may even be able to wear the Vacuum Bell whilst sleeping. When the Vacuum Bell is not worn the Pectus Clinic encourages a physically active lifestyle.
Difficult question. The evidence in the medical literature on how long VBT for Pectus Excavatum is required remains unclear and will depend on factors such as age when treatment started, severity and type of Pectus deformity; and most importantly commitment to a regular wearing schedule. An expectation of 1-2 years of VBT seems realistic.
Pectus deformity is often associated with other musculoskeletal problems, sometimes called 'pectus posture'. All patients as part of our follow-up pectus program will be shown specific exercises that will help other posture-related problems such as stooped shoulders and slouching. We strongly recommend regular and specific exercises.
Maybe. The Pectus Clinic works with the department of Physiotherapy at Spire St. Anthony’s and in conjunction with them have developed some specific exercise programs around musculoskeletal issues often seen in patients with Pectus deformities. If required, during your assessment a recommendation for additional physiotherapy will be made. This can then be booked to follow the VBT follow-up.
The VBT lasts around 1 to 2 years, and we recommend that you are seen 3 or 4 times after the first consultation to assess progress and give advice around VBT.
Ideally you should be seen in the first 12 weeks after VBT for a review. After this review, often (but not always) a further Pectus Clinic review will be offered typically at 6-9 months and finally at around 12-18 months following start of the Vacuum Bell program. Further appointments after that are usually not required.
Yes, please contact us if any worries, concerns or if you wish to check something. Often the best way is to simply email the pectus clinic. An email to us will be provided. We can arrange a Skype consultation if more helpful.
The overall cost of the VBT program is designed to be affordable and certainty when compared to the cost of dental bracing is comparable. For costs and payment methods please contact the Pectus Clinic administrator.
The Pectus Clinic was set up specifically to offer the best impartial advice for your pectus deformity. Because its run by doctors and other health care professionals who truly understand chest wall problems and pectus deformities specifically, we can provide all the information you need and help you decide what options you have.
If VBT is not the treatment for you, alternative treatments offered by the Pectus Clinic include corrective and non-corrective surgery. These treatments will be discussed with you following assessment.
Gallery
We take numerous measurements and photos before, during and after Vacuum Bell treatment as many of the problems we see centre around appearance. With the patient's permission we are happy to share our outcomes.
Results
It is important that we can show evidence that the Vacuum Bell treatment we offer and the results that we achieve are proven. We actively collect data to allow us to study, research and publish are outcomes.
Please click on the buttons below to see and read about patients verified experiences (in their own words) and testimonials (which generally include before and after treatment photos). The pectus clinic is very grateful to all the patients who provided feedback.
